[cmsmasters_row][cmsmasters_column data_width=”1/1″][cmsmasters_text]
ROP is an eye disease that could cause blindness in premature babies
While all non-COVID-19 services had come to a standstill during the pandemic, screening of newborns under the Karnataka Internet Assisted Diagnosis for Retinopathy of Prematurity (KIDROP) continued without any glitch. ROP is an eye disease that could cause blindness in premature babies.
KIDROP is the flagship tele-ROP programme started by Narayana Nethralaya in association with the Karnataka Government in 2009. It is a tele-medicine platform that benefits pre-term babies born in neo-natal intensive care units (NICUs) who do not have an ROP specialist to screen and treat the babies on time.
Addressing mediapersons in Bengaluru on the occasion of World Prematurity Day on November 17, Anand Vinekar, Professor and Head of Department of Pediatric Retina Service at Narayana Nethralaya Eye Institute, said no baby that required treatment for ROP was deprived of medical attention even during the COVID-19 pandemic.
“From April 2020 to December 2020, we screened 4,956 premature babies of which 232 needed treatment. All of them got treatment. Likewise, in 2021 from January to September 5, 412 babies were screened and 258 needing intervention got treatment,” he said.
Dr. Vinekar, who is the founding Programme Director of KIDROP, said around 3,000 online screening sessions were conducted per month during the pre-pandemic period. “However, during the first two months of the first wave of the pandemic, the number dropped to 682 due to lockdown and other restrictions. However, we managed to continue KIDROP and even treat newborns in rural areas using a very successful strategy. The number of new babies screened did not drop in 2020 when compared to 2019, making it a unique success story,” he said.
“During the peak of the pandemic, it was a challenge as special permissions had to be sought from the police and magistrates to shift babies across hospitals for treatment, as some government hospitals had been converted into dedicated COVID-19 facilities. But post-pandemic, the average has again risen to upwards of 2,000 screenings, and fortunately we have gone back to a ‘near- normal’ in most districts now,” the doctor explained.
Pointing out that COVID-19 modifications of the Indian ROP guidelines by the Centre helped in altering the screening profile, the doctor said, “We worked with the local police and the Bengaluru Police Commissioner to get special access for inter-district travel. ROP was declared as an emergency and special permissions were sought as newborns had to be screened within 48 hours. Moreover, as we had trained personnel for screening across the State, we managed with local screening by these personnel.”
K. Bhujang Shetty, chairman and managing director of Narayana Nethralaya, said all premature babies born and screened at government hospitals in Karnataka have been treated free of cost in the KIDROP programme since 2008.
“Through the programme, over two lakh newborn screening sessions have been done till date. More than 3,000 premature babies have been treated and saved from going blind. This is across 127 neo-natal centers spread across Karnataka. This is the single largest ROP cohort in the world that includes government district hospitals, private neo-natal units and medical college hospitals as well,” he said.
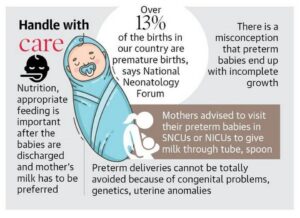
“In India 3.5 million (35 lakh) babies are born premature. Anywhere between 27% and 54% of these babies, who weigh less than two kilos, will get ROP. The disease burden is largest in countries like India. Of them, up to 15% will require treatment, which means nearly 1.5 lakh to 2.5 lakh pre-term babies in India require ROP treatment annually,” the doctor added.
As told by The Hindu
[/cmsmasters_text][/cmsmasters_column][/cmsmasters_row]